Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Pain Management
Overview
What is pain?
Pain is your body's way of warning you that something may be wrong. Pain can affect your emotions as well as your body. For example, if you put your hand on a hot stove, the pain lets you know right away that you're hurt and need to protect yourself. Pain can also make you feel irritable, anxious, or depressed. You may have pain from an injury, after surgery, or from a health problem like cancer, osteoarthritis, low back pain, headaches, or fibromyalgia.
Your body feels pain through nerves in your skin and organs. These nerve endings send pain signals to your brain.
Different ways people feel pain
Pain feels different for everyone. Something that doesn't bother one person might feel very bad to someone else.
Pain can feel sharp or dull. It may throb or burn. It may be in one part of your body, such as with a headache or a stomach ulcer. Or you may feel pain all over, like when your muscles ache from intense exercise or the flu.
Some pain may be so mild that you can ignore it until it goes away. But other pain may be so bad that you can't do your daily activities without medicine or other treatment.
Acute and chronic pain
Pain may last for a short time or a long time. It may come and go, or it may be constant.
Pain that starts quickly and lasts for a short time is called acute pain. Examples include pain from an injury, a headache, childbirth, or right after surgery.
Pain that goes on for months or years is called chronic pain. You may have this pain from an injury that doesn't heal or from a health problem like low back pain, very bad headaches, or nerve problems called neuropathy.
What are the different types of pain?
Different types of pain affect different parts of the body. Pain can affect:
- Muscles, bones, and joints.
It also affects the ligaments and tendons. This pain can happen from injuries or muscle strain. Health problems like osteoarthritis, rheumatoid arthritis, and fibromyalgia also can cause it.
- Nerves and the nervous system.
This type of pain happens because of pressure on nerves or damage to them from an injury or a health problem. Problems with the central nervous system can sometimes cause pain. Diabetes, shingles, and sciatica are examples of health problems that cause nerve pain.
- Organs.
Pain in your organs occurs because of injuries, infections, or other health problems. These problems include cancer, inflammatory bowel disease, irritable bowel syndrome, pelvic pain, and stomach ulcers.
You can have more than one kind of pain at the same time. For example, cancer can cause pain in your bones and your organs.
Reasons to Control Pain
Controlling your pain can help you to:
- Be active.
- Sleep.
- Cope better with your treatment for a health problem.
- Enjoy family and friends.
- Eat with pleasure.
- Heal faster after an injury or surgery.
Long-term pain that isn't controlled can take the joy from your life. You may not be able to work. Physical activity may be too painful or exhausting. You may have a hard time sleeping at night, which can make you tired and cranky. Your outlook on life may change and strain your relationships with family and friends. You may become depressed and anxious.
Controlling pain can help with all these things.
Treatments
Many different treatments can ease pain. How your pain is treated usually depends on how long you've been in pain and how bad it is. Often the best approach is a mix of treatments.
You and your doctor will work together to find ways to manage your pain so you can feel better and do more for yourself. But you still may have some pain.
If you have pain for a long time, your treatment may change over time.
Treatments other than medicines
Often people think of starting with a medicine to treat pain. But there are many non-medicine treatments that may be just as helpful. Your doctor may recommend these treatments with or without medicine. Non-medicine treatments may include:
- Physical treatments. This includes physical activity, massage, acupuncture, and heat or cold.
- Behavioral health treatments. This includes cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based stress reduction (MBSR).
- Mind-body treatments. This includes biofeedback, relaxation exercises, hypnosis, and yoga.
Medicines to treat pain
Several types of medicines can be used to treat pain. Most of them can treat more than one kind of pain. So you may need to try a couple of medicines to see which works best for you. Your doctor will work with you to find the right types and dosage of medicine. You may take more than one kind of medicine at the same time.
Medicines may include:
- Over-the-counter medicines. This may include acetaminophen (such as Tylenol) and nonsteroidal anti-inflammatory drugs (such as Advil).
- Anticonvulsants. This includes gabapentin (such as Neurontin) and topiramate (such as Topamax).
- Certain antidepressants. This includes duloxetine (such as Cymbalta), venlafaxine (such as Effexor), and amitriptyline.
- Opioids. This includes acetaminophen and hydrocodone (such as Norco) and morphine (such as Kadian).
Other options may include:
- Medicine you put on your skin. A variety of creams, gels, sprays, and patches may be used.
- Injections. Medicine may be injected into the spine, near the nerves that affects the painful area, or into the painful joint or joints.
Learn more
Knowing When Pain Is Worse
Pain can get worse slowly. So it can be hard to tell if your pain is getting worse, especially if you've had it for a while. But you can look for signs. You may notice that:
- You have new pain. It may feel different or be in a new area.
- Your pain treatment no longer works. Or maybe it doesn't work like it used to.
- Your medicine wears off too soon between doses.
- Your pain gets in the way of daily activities, like eating and sleeping.
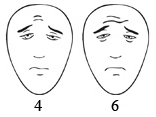
Using a pain scale and a pain diary can help you know how much pain you're having. A pain scale lets you rate your pain level as it changes. A pain diary is a record of your pain and how treatment is working. These tools also can help you tell your doctor what your pain feels like so that he or she can help you.
Learn more
Side Effects of Pain Medicines
All medicines have side effects. They vary depending on which medicine you take. Many side effects can be managed so that you can still take the medicine.
Side effects of over-the-counter medicines may include:
- Nausea or upset stomach.
- A rash.
- Heartburn.
- Liver damage (with high doses).
- Stomach or kidney problems (with long-term use).
Side effects of prescription medicines used for pain may include:
- Dizziness.
- Drowsiness or fatigue.
- Nausea or vomiting.
- Constipation.
- Getting sick if you stop taking the drug.
- Sleep problems.
- Loss of sexual desire.
Talk to your doctor if you have any side effects. Your doctor may change your dose or the type of medicine you take.
Learn more
Following a Treatment Plan
The best way to control your pain is to follow your treatment plan and give it time to work. The goal of your treatment plan is to be able to function and do the things you need to do, even if you still have some pain.
Some treatments may take a few days or weeks to improve your pain. You and your doctor can talk about how long you should keep using a medicine or other treatment.
Make the most of your pain medicines by following these rules.
- Take them on time (by the clock).
- Don't skip a dose or wait until you think you need it.
- Be prepared for breakthrough pain.
- You may find that taking your medicine works most of the time but that your pain flares up during extra activity or even for no clear reason. These flare-ups are called breakthrough pain.
- Your doctor can give you a prescription for fast-acting medicines that you can take for breakthrough pain.
Learn more
When to Call a Doctor
Only you can tell how much pain you have and whether it's getting better or worse. Talk to your doctor anytime you have new pain, your pain gets worse, or your treatment isn't controlling your pain.
Some people may think they're weak if they tell their doctor about their pain. Or they worry that they're bothering their doctor.
You're not weak. And you're not bothering the doctor. Your doctor wants to help you. But to help you, the doctor needs to know how you really feel.
Call your doctor if:
- Your pain gets worse or is out of control.
- You have stomach pain, an upset stomach, constipation, or heartburn that lasts or comes back.
- You don't get better as expected.
- You can't sleep because of pain.
- You are very worried or anxious or are feeling sad about your pain.
- Your pain medicine isn't working or you have trouble taking it.
Getting Support
You may have to lean on family and friends if you're getting over an injury or surgery or if you live with pain much of the time.
It can be hard sometimes to ask for help. But don't be afraid to reach out. Other people can help you—and they may be eager to help. Along with asking your family and friends, you can seek support from:
- A counselor.
A professional counselor can help you cope with pain, stress, and things that happen in your life. Counseling can help you understand and deal with an illness.
- Your doctor.
Find a doctor you trust and feel comfortable with. Be open and honest about your fears and concerns. Your doctor can help you get the right medical treatments, including counseling.
- Religious groups.
Religious or spiritual groups may help you meet people and get involved in the community. Some religious groups can help you get counseling or other social support services.
- Social groups.
You can meet new people and get involved in activities you enjoy.
- Community support groups.
In a support group, you can talk to others who have dealt with the same problems you have. You can encourage each other and learn ways of coping with your feelings.
Learn more
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.